Annex to the GLG Report: Towards specific commitments and action in the response to antimicrobial resistance
.tmb-479v.png?Culture=en&sfvrsn=72cdc10f_1)
Overview
Abbreviations
1. Background
The continued global challenge of antimicrobial resistance (AMR) across the One Health sectors is multifaceted, requiring the attention of a multitude of actors and stakeholders. Increased activities from global actors including the Quadripartite organizations (WHO, FAO, UNEP, and WOAH), the OECD, and the World Bank have sought to illuminate the continued challenges and act on the growing burden of AMR.
The IHME reported that, as of 2019, 1.27 million deaths were directly caused by bacterial AMR worldwide. At the regional level, the IHME estimated the all-age death rate attributable to resistance to be highest in western sub-Saharan Africa, at 27.3 deaths per 100,000 population (2). As for the European Economic Area (EEA), it was estimated that each year, more than 650,000 infections occur due to antibiotic resistant bacteria and more than 30,000 people die yearly as a result of these resistant infections (1). These negative health outcomes are estimated to cost the health sector more than €1 billion annually in EU/EEA countries alone (1).
In response to a request from the Global Leaders Group, the Quadripartite Joint Secretariat undertook an economic analysis to better understand the costs of AMR and the associated benefits of the AMR response across different sectors. The aim of this work is to inform global, regional, and country action on AMR response and to mobilize appropriate resources.
2. Methods
This work is composed of three primary components.
- A business-as-usual scenario to estimate the current and projected cost of AMR should no greater action be taken.
- A list of priority AMR interventions across sectors and the sub selection of a package of interventions for which cost-, and effectiveness-related data is available.
- An estimation of the return on investment (RoI) from implementing the package of interventions globally.
To validate the methodological approaches and to identify any missing data parameters, different groups of experts were consulted. In 2022, each organization of the Quadripartite, in addition to the World Bank, nominated an expert to participate in the meetings of the Core Group on the economics of AMR. The Core Group had oversight of each stage of this project. Additionally, the Quadripartite Technical Group on the economics of AMR (QTG-EA) was formed in early 2023, bringing together twenty selected experts across the globe to advise the Quadripartite organizations on the economic implications of tackling AMR across sectors. Members of QTG-EA provided feedback about the main assumptions, methodology, and inputs of the business-as-usual scenario, the selection of key AMR interventions, and investment case during four main meetings carried out during 2023 and January 2024. Finally, the regional of the Quadripartite organizations provided feedback in relation to the list of priority key AMR interventions and the methodology used to select them.
2.1 Estimating AMR losses: Business as usual scenario
The business-as-usual (BAU) scenario estimated the current and projected cost of AMR (in terms of healthcare expenditure and productivity loss) should no action be taken and was then used as the benchmark for the development of the investment case. It was estimated using a cost-of-illness approach with the OECD Strategic Public Health Planning (SPHeP) model -- an advanced systems modelling tool to predict health and economic outcomes (Figure 1). The version of the model that was used was explicitly adapted to the epidemiological characteristics of AMR (SPHeP-AMR) (4). The geographical scope of the analysis covered 14 regions, a combination of WHO geographic regions and of World Bank income categories (i.e. low, lower-middle, upper-middle, and high-income).
For each country or region, the model uses demographic and risk factor characteristics by age and gender (see Demographic module)(4). From these inputs, the model generates synthetic cohorts in which individuals are assigned demographic characteristics and risk factor profiles. Based on these profiles, individuals are characterized as having a certain annual risk of developing a disease of interest (see the Disease module). For each year of analysis, a cross-sectional representation of the population is used to calculate health status indicators such as the prevalence of the disease of interest, associated life expectancy and disability-adjusted life years (DALYs)(see Calculating disability weights)(4).
Figure 1. Graphical representation of the SPHeP model
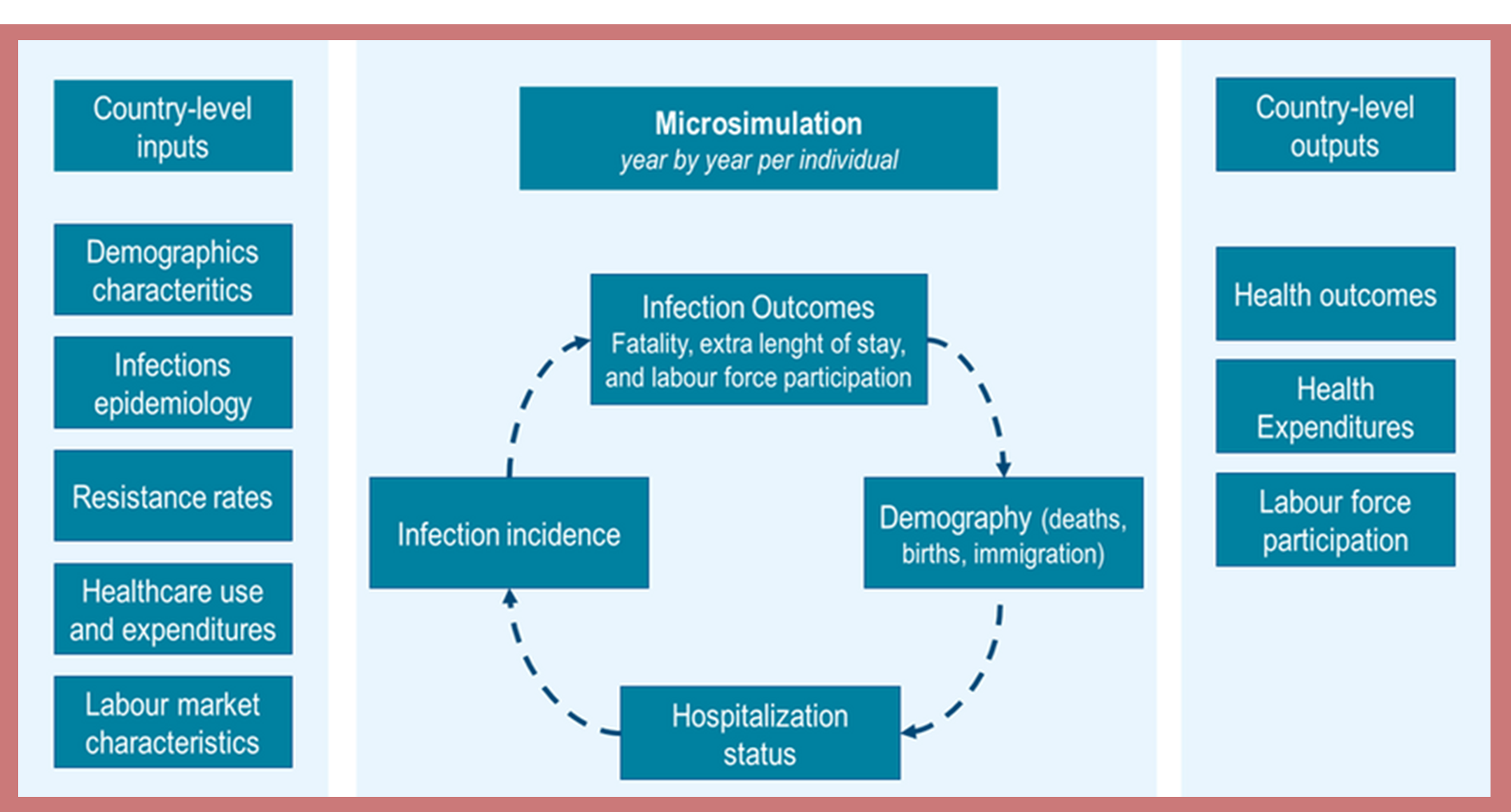
The model is designed to incorporate the economic impact of AMR from the societal perspective. Costs of infection treatment are estimated based on a per-case annual cost, which is extrapolated from national health-related expenditure data (see Healthcare costs). The overall cost of medical treatment is calculated by multiplying the number of hospitalizations attributed to the condition/pathogen by country-specific cost of treatment estimates.
The labor market module uses relative risks to connect disease status with the risks of absenteeism, presenteeism, early retirement and employment (see Labor market module). Changes in the workforce participation are assessed using the human capital approach, employing national average wages to calculate lost labor market outputs. A more detailed description of the SPHeP-AMR model is described in previously published reports by the OECD (4).
2.2. List of priority AMR interventions across sectors
To reach a list of priority AMR interventions to be modelled in the investment case, a multi-step consensus-driven approach was taken. To establish boundaries for the work and ensure consistency, key terminology and the scope of work were defined:
- Definition of key terminology: A priority AMR intervention is a broad (policy) intervention that seeks to answer one of the key objectives laid out in the Global Action Plan on AMR (5) or the Quadripartite One Health Joint Plan of Action (6). These interventions are also anticipated to be effective and have an economic impact. The “package” is the subset of interventions for which cost and effectiveness data was available, and therefore included in the investment analysis.
- Definition of sectors: Animal, human, environment, and plant were included. Interventions spanning multiple sectors were also considered.
- Applicability of interventions: The list of priority AMR interventions takes a global perspective yet acknowledges that countries are at different stages of readiness to address AMR. The list of priority AMR interventions is intended to be a menu for countries to digest and understand which interventions are relevant within and across sectors.
A targeted literature search of peer-reviewed articles (in PubMed) and publications from intergovernmental organizations, non-governmental organizations and research institutions was performed. In addition to the literature search, feedback was received on relevant evidence from the Quadripartite core group as well as from the Quadripartite Technical Group on the Economics of Antimicrobial Resistance (QTG-EA). Literature that met the inclusion criteria were selected and their information was extracted using a predesigned data extraction form. A summary of the included literature can be found in Appendix 1.
Appendix 2 provides an overview of each identified intervention per sector with a link to the reference.
2.3. Building the investment case
2.3.1. Investment case – General setting
The SPHeP-AMR model was run with the intention of simulating the impact of the policy package to tackle AMR. The package is assumed to be implemented in 2020 and its effect is calculated for the period spanning 2020-50. A multiplicative approach was used to combine the intervention effectiveness within the package. Economic effects focus on the change in healthcare expenditures and workforce participation. Population growth factors reported by the United Nations were considered for each region for future projections. No inflation factors were used. Undiscounted and discounted (3% and 6% annual discount rate) results are presented for both investments and benefits. The following formula was used to estimate the return on investment (RoI) from implementing the intervention package.
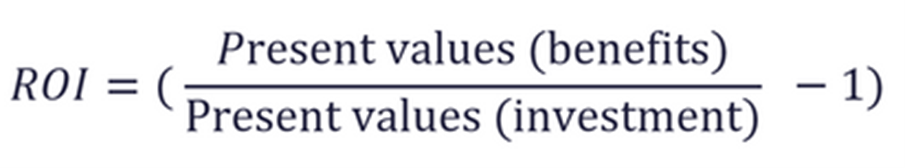
Where:
- RoI represents the return on investment. Values > 0 show that each invested unit gives a positive return, while values < 0 show a negative return.
- Present values (benefits) represent the present values for the intervention benefits (returns), throughout the analysis.
- Present values (investment) represent the present values for investments (implementation costs of interventions) throughout the analysis.
The base case assumed an equal distribution of investment for all years of analysis. A separate scenario assumed that 50% of the total investment occurs during the first year, and the rest (maintenance costs) is incurred in the remaining years. For this scenario, an annual discount rate of 3% was applied starting in the second year. The value of 50% was chosen based on the information reported for the WASH intervention investment (39). Additionally, results are presented for different subperiods within the time horizon of the analysis. Detailed information on the effectiveness of the intervention package, total investments and benefits is presented in sections that follow.
2.3.2. Investment case - Defining the final package of priority AMR interventions
For each of the 52 priority AMR interventions a targeted systematic literature review was conducted on cost-effectiveness or cost-analysis estimates spanning 2018 - 2023. Appendix 3 gives an overview of the identified studies. Each of the systematic reviews was then searched for specific primary studies that showed cost-effectiveness or cost-analysis estimates for the interventions of interest.
In a second step, targeted primary studies reporting cost and effectiveness data for each of the 52 priority AMR interventions were identified. The searches were performed in PubMed and specific grey literature databases and were limited to those published in English within the last 5 years. The aim was to capture any primary studies that were not captured by the systematic reviews. A detailed summary of search strategy for each intervention can be found in Appendix 4.
The literature searches combined identified effectiveness and cost information for 10 interventions out of 52 priority AMR interventions. However, on some cases, values for cost or effectiveness for more than one activity (component) were identified for a single intervention. A total of 13 components related to 10 interventions were finally selected for the RoI analysis. Table 1 summarizes the main characteristics of the final package. More details are provided in Appendix 5.
Baseline and target coverage values for each intervention were applied in the model. While baseline coverage was taken to vary in line with reported values, target intervention coverage was assumed to be similar for all regions. Appendix 6 reports information on the target coverage selected for each intervention (Table A6.1), as well as information about the effectiveness, population target, and impact for each intervention included in the package (Table A6.2).
Finally, to estimate the present value for investment (intervention costs), and in light of the complexity of conducting a micro costing for each intervention and each country/region, costs identified in the literature were extrapolated to the different regions, adjusting for PPP index values, using the most recent data from the World Bank. Details for each intervention are provided in Appendix 7.
Table 1. Final package of key AMR interventions for the RoI analysis
.png?sfvrsn=57a1393b_1)
3. Results
3.1. Expected losses due to AMR: Business as usual scenario
On average, a loss of 1.8 years in life expectancy could be attributed to AMR, ranging from 1.2 years for the upper-middle-income countries in the Western Pacific to 2.5 years for low and low-middle-income countries in the Eastern Mediterranean region.
Overall healthcare systems are expected to spend approximately US$ 412 billion per year between 2015 and 2035 due to AMR. Beyond the health sector, AMR is expected to depress economic activity through reduced participation in the workforce. Cumulative losses were estimated to be more than 68 million full-time equivalents (FTEs) every year, which can be considered as the number of individuals with a full-time job. If monetized using average national wages, this equates to a loss of US$ 443 billion per year.
3.2. Investment required to implement the package of AMR interventions
When considering the entire period of analysis (2020-2050) the total investment required for the intervention package across the regions was estimated to be approximately US$ 1,420.7 billion.
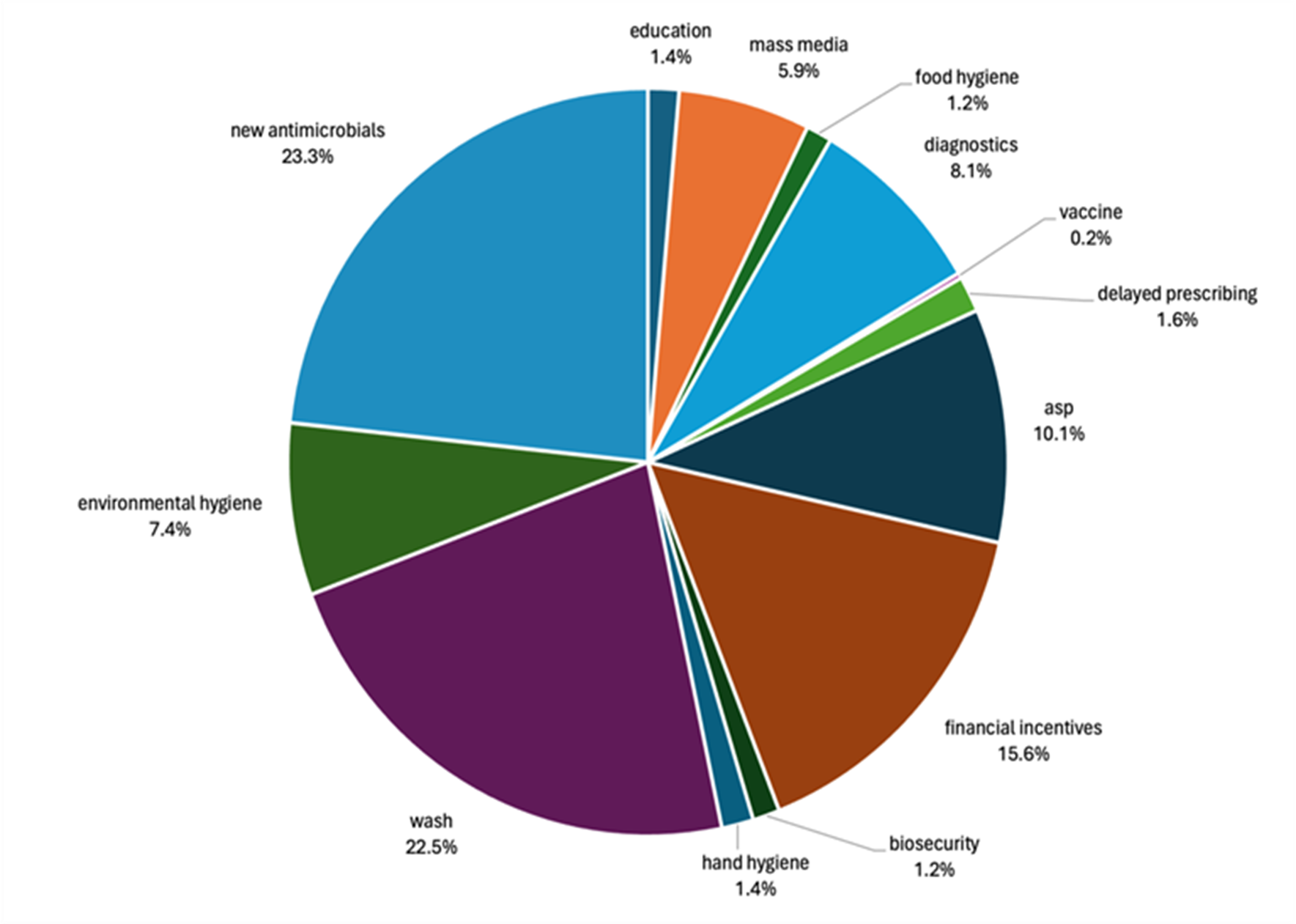
Figure 2 shows the distribution of total costs for the 13 intervention components included in the analysis. The new antibiotic incentive program represents more than a quarter (23.3%) of the total cost of the intervention package. Strengthened access to latrines and improved latrines (“WASH intervention”) represents 22.5% of the total investment.
Figure 2. Total investment required for the period of analysis 2020-2050 expressed in billion US$, 2020
3.3. Expected benefits from taking action: implementing the AMR Intervention package
Implementation of the package is estimated to produce significant savings to the healthcare systems across the regions. Cost savings related from reduced healthcare expenditure alone was estimated to be US$ 4,390 billion by 2035 and US$ 9,141 billion by 2050.
Financial gains produced by the package in terms of workforce participation were estimated to be US$ 3,293 billion by 2035 and US$ 9,939 billion by 2050.
3.4. Expected return-on-investment for implementing the package of AMR interventions
RoI results are presented for the base case and scenario analyses. When the longer period (2020-2050) is considered, the net RoI is estimated to be between 10.9 and 12.4, applying an annual discount rate of 6% and 0% respectively (Figure 3).
Figure 3: Estimated return on investment from implementing the package of AMR interventions globally (2020-2050)
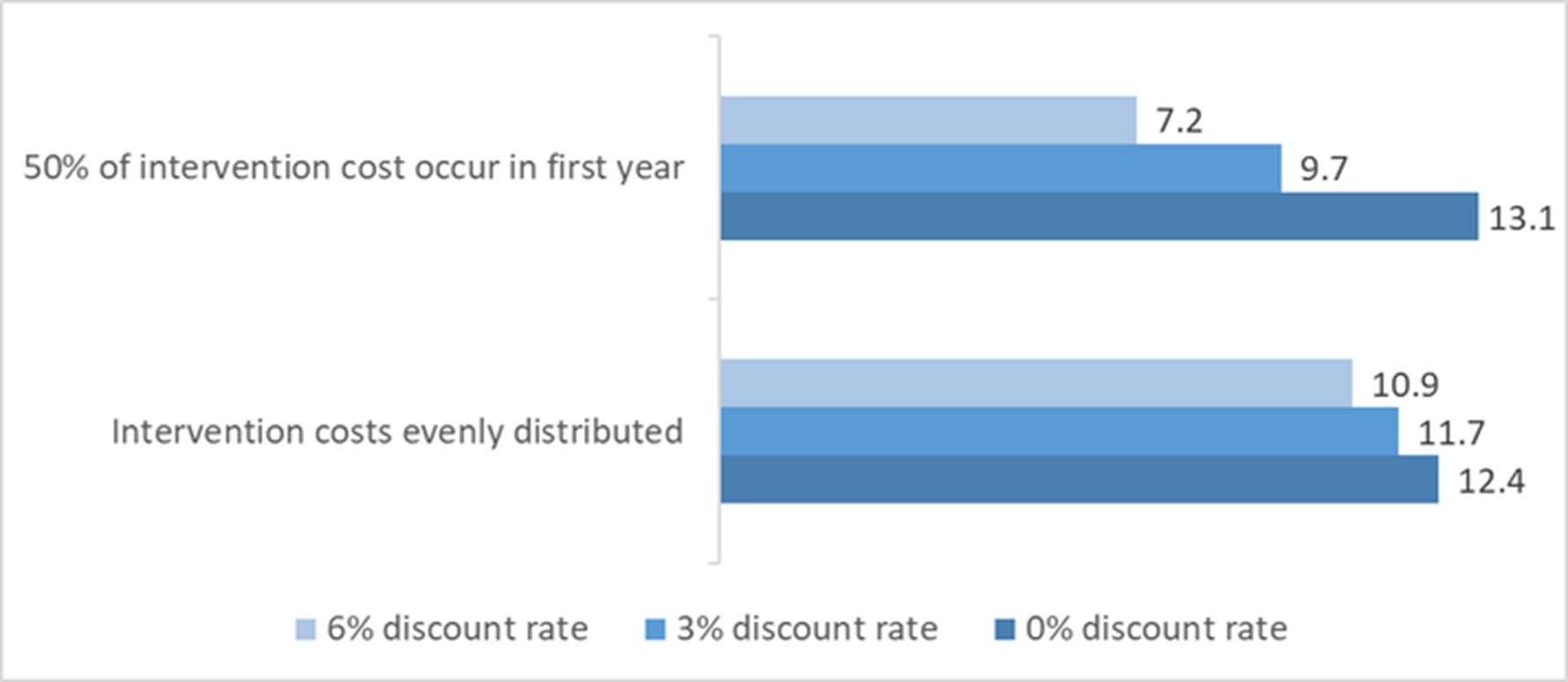
Note. These results suggest the returns that can be expected from every one dollar spent in implementing the package of AMR interventions.
4. Conclusions
.png?sfvrsn=6362f848_1)
The present document reports quantitative estimates of the disease burden that will be imposed by AMR in the decades to come, the ensuing economic implications, and the returns that can be made if we take greater action using a package of suitable interventions.
The study’s findings indicate that the economic burden of AMR is staggering and extends well beyond the healthcare sector. The long-term costs associated with treatment failures, increased healthcare use, and workforce losses due to illness are substantial. The business-as-usual case analysis found that, on average, a loss of 1.8 years in life expectancy could be attributed to AMR. In financial terms, US$ 412 billion of healthcare expenditures per year could be attributed to AMR. Also, concerning the workforce, a loss of more than 68 million full-time equivalents (FTE) could be attributed to AMR every year. While these losses are considerable, they comprise only part of the economic picture. Additional modelling is required to estimate losses deriving from the knock-on losses affecting the wider economy.
Total financial gains produced by the package are estimated to be US$ 3,293 billion for 2035 and US$ 9,939 billion for 2050. These projections highlight potential long-term economic advantages and substantial savings associated with implementing the proposed interventions. Even in the most conservative scenarios presented here, a global RoI of 7.2 was estimated for the period of analysis (2020-2050).
The findings from this investment case underscore the need for a collaborative, global effort to address AMR, with a focus on equitable distribution of resources to ensure that vulnerable populations countries benefit from these interventions. Developing countries often face resource constraints and are disproportionately affected by infectious diseases. Allocating funds to AMR interventions such as strengthening healthcare infrastructure, promoting antimicrobial stewardship, and improving awareness and understanding of AMR can yield significant health and financial benefits, breaking the cycle of transmission and contributing to global health security.
The study also emphasizes the importance of a One Health approach, recognizing the interconnectedness of human, animal, and environmental health. By investing in interventions that promote responsible antimicrobial use in both human healthcare and agriculture, we can create a holistic strategy that addresses the root causes of AMR and reduces the emergence and spread of resistant pathogens.
The present study has limitations. Given the lack of information on the effectiveness and costs of interventions from studies conducted in LMICs, much of the information obtained comes from high-income countries. While an adjustment has been made for PPP index values to extrapolate costs to low- and middle-income regions, effectiveness values have been assumed to be the same. However, region-specific data on the current coverage (business-as-usual intervention coverage) was used for each intervention.
Overall this study offers a framework within which parameters can be refined as more data become available. It can also help serve as a baseline to track changes in the economic outlook as countries move forward in National Action Plan implementation.
In conclusion, the findings of this investment case make a compelling argument for the prioritization of interventions to tackle AMR across sectors. The high RoI highlights the transformative potential of targeted interventions in mitigating the financial and health consequences of AMR. Policymakers are urged to heed these findings and allocate resources strategically to ensure a sustainable and resilient future in the face of the growing threat posed by AMR.
Supplementary Material
Appendix 1. Overview of evidence – Literature review
Table A1.1: Overview of evidence.
| Study | Title | Overview and Key Findings |
| OECD & WHO, 2022 | Addressing the Burden of Infections and Antimicrobial Resistance Associated with Health Care | The report discussed various interventions suggested by the organization in addressing antimicrobial resistance. Evidence behind the interventions suggested were also provided. |
| Morel et al, 2020 | A one health framework to estimate the cost of antimicrobial resistance | The study created a costing framework that may be utilized by first identifying the most common antimicrobial resistance pathogens and how the epidemiologic pattern of AMR is. This was followed by analyzing the probabilities for each sector (human health, animal health, and others). |
| World Bank, 2021, unpublished | "Stopping the Silent Epidemic: An Operational Framework for Addressing Antimicrobial Resistance" Working Draft | The document presented a framework in looking at various interventions to address antimicrobial resistance. It divided interventions into AMR-sensitive and AMR-specific. |
| WHO & World Bank, 2022 | Sustaining Action Against Antimicrobial Resistance: A Case Series of Country Experiences | The report presented case series of several countries, mostly from LMICs with their strengths and weaknesses in implementing their national action plan against antimicrobial resistance as pushed by member countries. |
| WHO, 2019 | Global Antimicrobial Resistance Surveillance System (GLASS) | The GLASS report was created to boost AMR surveillance among member countries. This was thus a report describing it and discussing key points on surveillance with regards to national action plans of countries. |
| FAO, 2022 | Tackling Antimicrobial Use and Resistance in Food-producing Animals: Lessons Learned in the United Kingdom | The FAO discussed interventions within the animal health realm in addressing antimicrobial resistance using the United Kingdom as a case study for discussion on national plans for AMR. |
| OECD & WHO, 2019 | Challenges to Tackling Antimicrobial Resistance | The joint report presented interventions aimed at tackling antimicrobial resistance. It provided a good background on infection control and different approaches to address AMR. |
| WHO, 2021 | Comprehensive Review of the WHO Global Action Plan (GAP) on Antimicrobial Resistance | The document presented indicators per GAP objective identified to monitor and evaluate efforts for AMR. |
| WHO, 2022 | People centered framework for addressing AMR ppt | Overview of interventions for human health |
| Jit et al, 2020 | Quantifying the economic cost of antibiotic resistance and the impact of related interventions: rapid methodological review, conceptual framework and recommendations for future studies | The study proposed a conceptual framework for antibiotic resistance. |
| UNEP, 2022 | Environmental Dimensions of Antimicrobial Resistance: Summary for Policymakers | The paper presents environmental impacts of AMR and the causes of the development and spread of resistance in the environment, including the gaps in understanding those impacts and causes. |
| FAO, 2021 | The FAO Action Plan on Antimicrobial Resistance 2021-2025 | This FAO Action Plan on AMR 2021–2025 sets out the five objectives that guide the programming of FAO activities: 1. Increasing stakeholder awareness and engagement 2. Strengthening surveillance and research 3. Enabling good practices 4. Promoting responsible use of antimicrobials 5. Strengthening governance and allocating resources sustainably |
| OECD, 2018 | Stemming the Superbug Tide: Just a Few Dollars More | In this report, OECD used advanced techniques, including machine learning, ensemble modelling and a microsimulation model, to provide support for policy action in the human health sector. |
| World Bank, 2017 | Drug Resistant Infections: A Threat to Our Economic Future | This report examines the economic and development consequences of antimicrobial resistance (AMR), using the World Bank Group economic simulation tools to put a price tag on AMR’s destructive impacts on the global economy from 2017 through 2050, if adequate measures aren’t taken to contain the AMR threat. |
| Al-Haboubi et al, 2020 | Views of health care professionals and policy-makers on the use of surveillance data to combat antimicrobial resistance | Identified the extent of the use of AMR data to the perceived needs of healthcare professionals and policymakers |
| PIRU RVC, 2019 | Impact of guidelines and recommendations on the level and patterns of antimicrobial use in livestock and companion animals: Systematic Review | Explored guidelines in Europe and analyzed their impact on AMR relating to farm animals and companion animals |
| EFSA and EMA, 2016 | EMA and EFSA Joint Scientific Opinion on measures to reduce the need to use antimicrobial agents in animal husbandry in the European Union, and the resulting impacts on food safety (RONAFA) | Assessment and recommendations on AMR interventions in the European region |
| OECD, 2019 | Evaluating the economic benefits and costs of antimicrobial use in food producing animals | Evaluated on an economic perspective and provided interventions to promote AMR action |
Appendix 2. Package of key AMR interventions per sector (long-list)
Table A2.1. Package of key AMR interventions per sector (long-list): Animal, Human, Environment and Plant sectors
| Objectives | Animal | Human | Environment | Plant |
| Improve awareness and understanding of AMR | Improve awareness, education, and behavior/perception change programs incl. learning experiences for farmers, veterinarians, veterinarian students, pet owners, regulators, and the general public. | AMR awareness raising, education and behavior change of health workers and the community. |
| Communicate with, educate, and provide training to farmers on AMR, integrated pest management (IPM), and the appropriate use and disposal of pesticides / herbicides/ molluscicides. |
| Strengthen knowledge and evidence-based through surveillance and research |
|
|
| National surveillance of AMR data in food and agriculture and AMU data in crops through enrolling in the International FAO Antimicrobial Resistance Monitoring (InFARM). |
| Reduce the incidence of infection through effective sanitation, hygiene, and infection prevention measures. |
|
|
| Incentivize farm assurance or certification benchmarking schemes in farms. |
| Optimize the use of antimicrobial medicines in human and animal health |
|
|
|
|
| Increase investment in new medicines, diagnostic tools, vaccines and other interventions |
| Research into new antimicrobials, diagnostics and vaccines for AMR and behavioral and implementation science. |
| - |
Abbreviations: AMR = Antimicrobial Resistance, AMU = Antimicrobial use, BSL = Biological Safety Level, INFARM = International FAO Antimicrobial Resistance Monitoring, IPC = Infection, Prevention, Control, IPM = integrated pest management, OTC = over-the-counter, RENOFARM = Reduce the Need for Antimicrobials on Farms, WASH = Water, Sanitation and Hygiene
Table A2.2. Package of key AMR interventions across sectors (One Health, cross-cutting interventions)
| Objectives | Cross-cutting interventions |
|---|---|
| Enhance policy, legislation, advocacy and financing. |
|
| Strengthen organizational development, implementation and sectoral integration |
|
| Implement data, evidence, and knowledge |
|
Abbreviations: AMR = Antimicrobial Resistance, ESG = Environmental, Social, and Governance, HP=CIAs = Highest Priority Critically Important Antibiotics (HP-CIAs), JPA = Joint Plan of Action, NAP = National Action Plan, OH = One Health, PPE = Personal Protective Equipment, QJS = Quadripartite
* This includes the intervention “AMR advocacy, governance, and accountability in the human health sector in collaboration with other sectors.” As mentioned in the WHO People-Centred Framework
Appendix 3. Systematic literature reviews reporting cost-effectiveness or cost-analysis information of AMR interventions
Table A3.1. Overview of systematic literature reviews (2018-2023) reporting cost-effectiveness or cost-analysis information of AMR interventions
| Human | One Health |
| Ananthakrishnan A, et al. A protocol for a systematic literature review of economic evaluation studies of interventions to address antimicrobial resistance, 2021 | Naylor, NR, et al. Quantitatively evaluating the cross-sectoral and One Health impact of interventions: A scoping review and case study of antimicrobial resistance, 2020 |
| Poudel AN, et al. The economic burden of antibiotic resistance: A systematic review and meta-analysis, 2023 | Quadripartite One Health Return on Investment |
| Befikadu L Wubishet et al. Economic evaluation of antimicrobial stewardship in primary care: a systematic review and quality assessment, 2022. | Aluzaite, K, et al. Economic evaluation of interventions to reduce antimicrobial resistance: a systematic literature review of methods. Unpublished. |
| Painter, C., Faradiba, D., Chavarina, K.K. et al. A systematic literature review of economic evaluation studies of interventions impacting antimicrobial resistance, 2023. | |
| D'hulster E, et al. Cost-effectiveness of point-of-care interventions to tackle inappropriate prescribing of antibiotics in high- and middle-income countries: a systematic review, 2023. | |
| Carla Cuevas et al., Improving antibiotic use through behaviour change: a systematic review of interventions evaluated in low- and middle-income countries, 2021. | |
| Nathwani, D. et al. Value of hospital antimicrobial stewardship programs [ASPs]: a systematic review, (2019) |
Appendix 4. Search strategies of the targeted review literature conducted
a.1. Systematic reviews
Search strategy (PubMed):
(Drug Resistance, Microbial"[MeSH Terms] OR Antimicrobial resistance* [tiab] OR Antibiotic resistance* [tiab]) AND (costs and cost analysis [MeSH] OR cost savings [MeSH] OR cost-benefit analysis [MeSH] OR economic evaluation [tiab] OR cost analysis [tiab] OR cost-effectiveness [tiab] OR cost control [tiab] OR cost efficiency analysis [tiab] OR cost-effectiveness analysis [MeSH] ) AND (systematic review[Publication Type])
Filter: Last 5 years;
b.1. Human
b.1.1. AMR awareness raising, education and behavior change of health workers and the community.
Search strategy (PubMed):
("Drug Resistance, Microbial"[MeSH Terms] OR Antimicrobial resistance* [tiab] OR Antibiotic resistance* [tiab]) AND (Awareness [tiab] OR Education*[tiab] OR Behavior change[tiab]) AND (costs and cost analysis [MeSH] OR cost savings [MeSH] OR cost-benefit analysis [MeSH] OR economic evaluation [tiab] OR cost analysis [tiab] OR cost-effectiveness [tiab] OR cost control [tiab] OR cost efficiency analysis [tiab] OR cost-effectiveness analysis [MeSH])
Filter: Last 5 years; Full Text.
b.1.2 National AMR surveillance network to generate quality data to inform patient care and action on AMR.
Search strategy (PubMed):
("Drug Resistance, Microbial"[MeSH Terms] OR Antimicrobial resistance* [tiab] OR Antibiotic resistance* [tiab]) AND Surveillance [tiab] AND (costs and cost analysis [MeSH] OR cost savings [MeSH] OR cost-benefit analysis [MeSH] OR economic evaluation [tiab] OR cost analysis [tiab] OR cost-effectiveness [tiab] OR cost control [tiab] OR cost efficiency analysis [tiab] OR cost-effectiveness analysis [MeSH])
Filter: Last 5 years; Full Text.
b.1.3 Antimicrobial consumption and use surveillance to inform patient care and action on AMR.
Search strategy (PubMed):
("Drug Resistance, Microbial"[MeSH Terms] OR Antimicrobial resistance* [tiab] OR Antibiotic resistance* [tiab]) AND (Surveillance [tiab] OR consumption [tiab]) AND (costs and cost analysis [MeSH] OR cost savings [MeSH] OR cost-benefit analysis [MeSH] OR economic evaluation [tiab] OR cost analysis [tiab] OR cost-effectiveness [tiab] OR cost control [tiab] OR cost efficiency analysis [tiab] OR cost-effectiveness analysis [MeSH])
Filter: Last 5 years; Full Text.
Results: none met the inclusion criteria.
b.1.4. Implementation of infection, prevention and control (IPC) core components to mitigate AMR.
Search strategy (PubMed):
("Drug Resistance, Microbial"[MeSH Terms] OR Antimicrobial resistance* [tiab] OR Antibiotic resistance* [tiab]) AND (infect* control [tiab] OR infect* prevention [tiab]) AND (costs and cost analysis [MeSH] OR cost savings [MeSH] OR cost-benefit analysis [MeSH] OR economic evaluation [tiab] OR cost analysis [tiab] OR cost-effectiveness [tiab] OR cost control [tiab] OR cost efficiency analysis [tiab] OR cost-effectiveness analysis [MeSH])
Filter: Last 5 years; Full Text.
b.1.5. Universal access to improved WASH and waste management to mitigate AMR.
Search strategy (PubMed):
("Drug Resistance, Microbial"[MeSH Terms] OR Antimicrobial resistance* [tiab] OR Antibiotic resistance* [tiab]) AND (WASH [tiab] OR waste [tiab]) AND (costs and cost analysis [MeSH] OR cost savings [MeSH] OR cost-benefit analysis [MeSH] OR economic evaluation [tiab] OR cost analysis [tiab] OR cost-effectiveness [tiab] OR cost control [tiab] OR cost efficiency analysis [tiab] OR cost-effectiveness analysis [MeSH])
Filter: Last 5 years; Full Text.
b.1.6. Quality laboratory system and diagnostic stewardship to enable clinical bacteriology and mycology testing.
Search strategy (PubMed):
("Drug Resistance, Microbial"[MeSH Terms] OR Antimicrobial resistance* [tiab] OR Antibiotic resistance* [tiab]) AND (test* [tiab]) AND (costs and cost analysis [MeSH] OR cost savings [MeSH] OR cost-benefit analysis [MeSH] OR economic evaluation [tiab] OR cost analysis [tiab] OR cost-effectiveness [tiab] OR cost control [tiab] OR cost efficiency analysis [tiab] OR cost-effectiveness analysis [MeSH])
Filter: Last 5 years; Full Text.
b.1.7. Access to vaccines and expanded immunisation to manage AMR.
Search strategy (PubMed):
("Drug Resistance, Microbial"[MeSH Terms] OR Antimicrobial resistance* [tiab] OR Antibiotic resistance* [tiab]) AND (vaccin* [tiab] OR immunisation [tiab]) AND (costs and cost analysis [MeSH] OR cost savings [MeSH] OR cost-benefit analysis [MeSH] OR economic evaluation [tiab] OR cost analysis [tiab] OR cost-effectiveness [tiab] OR cost control [tiab] OR cost efficiency analysis [tiab] OR cost-effectiveness analysis [MeSH])
Filter: Last 5 years; Full Text.
b.1.8. Up-to-date evidence-based treatment guidelines and antimicrobial stewardship programmes.
Search strategy (PubMed):
("Drug Resistance, Microbial"[MeSH Terms] OR Antimicrobial resistance* [tiab] OR Antibiotic resistance* [tiab]) AND (evidence-based [tiab] OR guideline* [tiab]) AND (costs and cost analysis [MeSH] OR cost savings [MeSH] OR cost-benefit analysis [MeSH] OR economic evaluation [tiab] OR cost analysis [tiab] OR cost-effectiveness [tiab] OR cost control [tiab] OR cost efficiency analysis [tiab] OR cost-effectiveness analysis [MeSH])
Filter: Last 5 years; Full Text.
b.1.9. Implementation of regulation to restrict non-prescription antimicrobial sales.
Search strategy (PubMed):
("Drug Resistance, Microbial"[MeSH Terms] OR Antimicrobial resistance* [tiab] OR Antibiotic resistance* [tiab]) AND (regulat* [tiab] OR prescription* [tiab]) AND (costs and cost analysis [MeSH] OR cost savings [MeSH] OR cost-benefit analysis [MeSH] OR economic evaluation [tiab] OR cost analysis [tiab] OR cost-effectiveness [tiab] OR cost control [tiab] OR cost efficiency analysis [tiab] OR cost-effectiveness analysis [MeSH])
Filter: Last 5 years; Full Text.
b.1.10. Uninterrupted supply of essential health products for AMR.
Search strategy (PubMed):
("Drug Resistance, Microbial"[MeSH Terms] OR Antimicrobial resistance* [tiab] OR Antibiotic resistance* [tiab]) AND (accessibility [tiab] OR affordability [tiab]) AND (costs and cost analysis [MeSH] OR cost savings [MeSH] OR cost-benefit analysis [MeSH] OR economic evaluation [tiab] OR cost analysis [tiab] OR cost-effectiveness [tiab] OR cost control [tiab] OR cost efficiency analysis [tiab] OR cost-effectiveness analysis [MeSH])
Filter: Last 5 years; Full Text.
b.1.11. AMR diagnosis and management health services are made affordable for all.
Search strategy (PubMed):
("Drug Resistance, Microbial"[MeSH Terms] OR Antimicrobial resistance* [tiab] OR Antibiotic resistance* [tiab]) AND (accessibility [tiab] OR affordab* [tiab]) AND (costs and cost analysis [MeSH] OR cost savings [MeSH] OR cost-benefit analysis [MeSH] OR economic evaluation [tiab] OR cost analysis [tiab] OR cost-effectiveness [tiab] OR cost control [tiab] OR cost efficiency analysis [tiab] OR cost-effectiveness analysis [MeSH])
Filter: Last 5 years; Full Text.
b.1.12. Research into new antimicrobials, diagnostics and vaccines for AMR and behavioural and implementation science.
Search strategy (PubMed):
("Drug Resistance, Microbial"[MeSH Terms] OR Antimicrobial resistance* [tiab] OR Antibiotic resistance* [tiab]) AND (new [tiab] OR novel [tiab]) AND (costs and cost analysis [MeSH] OR cost savings [MeSH] OR cost-benefit analysis [MeSH] OR economic evaluation [tiab] OR cost analysis [tiab] OR cost-effectiveness [tiab] OR cost control [tiab] OR cost efficiency analysis [tiab] OR cost-effectiveness analysis [MeSH])
Filter: Last 5 years; Full Text.
b.2.1. Improve awareness, education, and behaviour/perception change programs incl. learning experiences for farmers, veterinarians, veterinarian students, pet owners, regulators, and the general public.
Search strategy (PubMed):
("Drug Resistance, Microbial"[MeSH Terms] OR Antimicrobial resistance* [tiab] OR Antibiotic resistance* [tiab]) AND (farmer*[tiab] OR veterina*[tiab] OR pet owners[tiab] OR regulators[tiab] OR general public [tiab]) (costs and cost analysis [MeSH] OR cost savings [MeSH] OR cost-benefit analysis [MeSH] OR economic evaluation [tiab] OR cost analysis [tiab] OR cost-effectiveness [tiab] OR cost control [tiab] OR cost efficiency analysis [tiab] OR cost-effectiveness analysis [MeSH])
Filter: Last 5 years; Full Text.
b.2.2. National AMR surveillance to inform development and allow assessment of effectiveness of interventions and policies at national level.
Search strategy (PubMed):
("Drug Resistance, Microbial"[MeSH Terms] OR Antimicrobial resistance* [tiab] OR Antibiotic resistance* [tiab]) AND Surveillance [tiab] AND (costs and cost analysis [MeSH] OR cost savings [MeSH] OR cost-benefit analysis [MeSH] OR economic evaluation [tiab] OR cost analysis [tiab] OR cost-effectiveness [tiab] OR cost control [tiab] OR cost efficiency analysis [tiab] OR cost-effectiveness analysis [MeSH])
Filter: Last 5 years; Full Text.
b.2.3. National AMU surveillance to inform development and allow assessment of effectiveness of interventions and policies at national level.
Search strategy (PubMed):
("Drug Resistance, Microbial"[MeSH Terms] OR Antimicrobial resistance* [tiab] OR Antibiotic resistance* [tiab]) AND (Use [tiab]) AND (costs and cost analysis [MeSH] OR cost savings [MeSH] OR cost-benefit analysis [MeSH] OR economic evaluation [tiab] OR cost analysis [tiab] OR cost-effectiveness [tiab] OR cost control [tiab] OR cost efficiency analysis [tiab] OR cost-effectiveness analysis [MeSH])
Filter: Last 5 years; Full Text; Species: Other Animals.
b.2.4. Implementation of biosecurity measures to prevent the introduction and spread of disease in farms.
Search strategy (PubMed):
biosecurity [tiab] AND farm*[tiab] AND (costs and cost analysis [MeSH] OR cost savings [MeSH] OR cost-benefit analysis [MeSH] OR economic evaluation [tiab] OR cost analysis [tiab] OR cost-effectiveness [tiab] OR cost control [tiab] OR cost efficiency analysis [tiab] OR cost-effectiveness analysis [MeSH])
Filter: Last 5 years; Full Text.
b.2.5. Ensure good animal husbandry and farm management practices linked to the Five Freedoms of animal welfare.
Search strategy (PubMed):
("Drug Resistance, Microbial"[MeSH Terms] OR Antimicrobial resistance* [tiab] OR Antibiotic resistance* [tiab]) AND (farm [tiab] OR animal [tiab]) AND (costs and cost analysis [MeSH] OR cost savings [MeSH] OR cost-benefit analysis [MeSH] OR economic evaluation [tiab] OR cost analysis [tiab] OR cost-effectiveness [tiab] OR cost control [tiab] OR cost efficiency analysis [tiab] OR cost-effectiveness analysis [MeSH])
Filter: Last 5 years; Full Text.
b.2.6. Increase veterinary laboratory capacity (including ability to transport, store and process samples appropriately).
Search strategy (PubMed):
("Drug Resistance, Microbial"[MeSH Terms] OR Antimicrobial resistance* [tiab] OR Antibiotic resistance* [tiab]) AND (veterin* [tiab] OR labo* [tiab]) AND (costs and cost analysis [MeSH] OR cost savings [MeSH] OR cost-benefit analysis [MeSH] OR economic evaluation [tiab] OR cost analysis [tiab] OR cost-effectiveness [tiab] OR cost control [tiab] OR cost efficiency analysis [tiab] OR cost-effectiveness analysis [MeSH])
Filter: Last 5 years; Full Text.
b.2.7. Promotion of use of viable / natural alternatives (e.g., prebiotic, probiotic) to reduce AMU (e.g., vaccines in salmon farming or alternatives to growth promotion).
Search strategy (PubMed):
("Drug Resistance, Microbial"[MeSH Terms] OR Antimicrobial resistance* [tiab] OR Antibiotic resistance* [tiab]) AND (Antimicrobial use [tiab]) AND (costs and cost analysis [MeSH] OR cost savings [MeSH] OR cost-benefit analysis [MeSH] OR economic evaluation [tiab] OR cost analysis [tiab] OR cost-effectiveness [tiab] OR cost control [tiab] OR cost efficiency analysis [tiab] OR cost-effectiveness analysis [MeSH])
Filter: Last 5 years; Full Text.
b.2.8. Create prescribing guidelines and stewardship programs at national level for targeted AMU including indication, line of therapy, dose, administration route and course of treatment of antimicrobials (e.g. switch from broad-spectrum to appropriate narrow-spectrum antimicrobial substances) with no perverse incentives (e.g. delinking prescribing with remuneration).
Search strategy (PubMed):
(Antimicrobial use [tiab]) AND (costs and cost analysis [MeSH] OR cost savings [MeSH] OR cost-benefit analysis [MeSH] OR economic evaluation [tiab] OR cost analysis [tiab] OR cost-effectiveness [tiab] OR cost control [tiab] OR cost efficiency analysis [tiab] OR cost-effectiveness analysis [MeSH])
Filter: Last 5 years; Full Text.
b.2.9. Phasing out over-the-counter (OTC) should be coupled with ensuring the availability of quality and affordable antibiotics.
Search strategy (PubMed):
("Drug Resistance, Microbial"[MeSH Terms] OR Antimicrobial resistance* [tiab] OR Antibiotic resistance* [tiab]) AND (accessibility [tiab] OR affordab* [tiab]) AND (costs and cost analysis [MeSH] OR cost savings [MeSH] OR cost-benefit analysis [MeSH] OR economic evaluation [tiab] OR cost analysis [tiab] OR cost-effectiveness [tiab] OR cost control [tiab] OR cost efficiency analysis [tiab] OR cost-effectiveness analysis [MeSH])
Filter: Last 5 years; Full Text.
b.2.10. Ensure accessibility and affordability of AMR diagnostics.
Search strategy (PubMed):
("Drug Resistance, Microbial"[MeSH Terms] OR Antimicrobial resistance* [tiab] OR Antibiotic resistance* [tiab]) AND (accessibility [tiab] OR affordab* [tiab]) AND (costs and cost analysis [MeSH] OR cost savings [MeSH] OR cost-benefit analysis [MeSH] OR economic evaluation [tiab] OR cost analysis [tiab] OR cost-effectiveness [tiab] OR cost control [tiab] OR cost efficiency analysis [tiab] OR cost-effectiveness analysis [MeSH])
Filter: Last 5 years; Full Text.
b.2.11. Research and development of novel, cost-effective, and affordable vaccines.
Search strategy (PubMed):
("Drug Resistance, Microbial"[MeSH Terms] OR Antimicrobial resistance* [tiab] OR Antibiotic resistance* [tiab]) AND (new [tiab] OR novel [tiab]) AND (costs and cost analysis [MeSH] OR cost savings [MeSH] OR cost-benefit analysis [MeSH] OR economic evaluation [tiab] OR cost analysis [tiab] OR cost-effectiveness [tiab] OR cost control [tiab] OR cost efficiency analysis [tiab] OR cost-effectiveness analysis [MeSH])
Filter: Last 5 years; Full Text.
b.2.12. Develop veterinary/animal/farm-appropriate diagnostics.
Search strategy (PubMed):
("Drug Resistance, Microbial"[MeSH Terms] OR Antimicrobial resistance* [tiab] OR Antibiotic resistance* [tiab] OR Antimicrobial use[tiab]) AND (diag*[tiab]) AND (animal*[tiab] OR farm*[tiab] OR veterin*[tiab]) AND (costs and cost analysis [MeSH] OR cost savings [MeSH] OR cost-benefit analysis [MeSH] OR economic evaluation [tiab] OR cost analysis [tiab] OR cost-effectiveness [tiab] OR cost control [tiab] OR cost efficiency analysis [tiab] OR cost-effectiveness analysis [MeSH])
Filter: Last 5 years; Full Text.
b.3. Environment
b.3.1. Education and awareness of key source pollution emitters for appropriate and point-source waste prevention and treatment, and protection of source waters.
Search strategy (grey literature, Google Scholar):
Cost AND pollution emitters AND education OR awareness AND AMR OR AMU
Filter: Lat 5 years; first three pages.
b.3.2. Education and awareness of environmental and other relevant-sector authorities on the role of the environment t in AMR development, transmission and spread.
Search strategy (grey literature, Google Scholar):
Cost AND environment AND education OR awareness AND AMR OR AMU
Filter: Lat 5 years; first three pages.
b.3.3. Implement systems for transparent and swift collection and reporting of the production, sales, use, and disposal of unused antimicrobials.
Search strategy (grey literature, Google Scholar):
Cost AND unused antimicrobials AND education OR awareness AND environment
Filter: Lat 5 years; first three pages.
b.3.4. Integrate environmental monitoring data (e.g., from monitoring of surface water, solid waste, and airborne particulate matter) with existing AMR surveillance and pollutants data.
Search strategy (grey literature, Google Scholar):
Cost AND environment AND data OR surveillance AND AMR OR AMU
Filter: Lat 5 years; first three pages.
b.3.5. Document the safety of bioproducts (e.g., biofertilizers, bioplastics, biosolid and manure applications, and plant growth promoters) and novel agricultural practices, as well as key sources of pollution that indicate an impact on AMR in the environment.
Search strategy (grey literature, Google Scholar):
Cost AND environment AND safety bioproduct AND AMR OR AMU
Filter: Lat 5 years; first three pages.
b.3.6. Improve integrated water management and promote water, sanitation, and hygiene (WASH) to limit the development and spread of AMR in the environment as well as to reduce infections and need for antimicrobials.
Search strategy (grey literature, Google Scholar):
Cost AND environment AND WASH OR water AND AMR OR AMU
Filter: Lat 5 years; first three pages.
b.3.7. Ensure safe and sustainable disposal and treatment of antimicrobials and hazardous waste from healthcare facilities, pharmacies, veterinarian centers, animal and crop production, and households (e.g., creating, strengthening and promoting take-back programs).
Search strategy (grey literature, Google Scholar):
Cost AND environment AND waste AND AMR OR AMU
Filter: Lat 5 years; first three pages.
b.3.8. Implement an integrated zoonotic disease surveillance system to detect disease emergence in human/animal population.
Search strategy (grey literature, Google Scholar):
Cost AND zoonotic AND disease AND AMR OR AMU
Filter: Lat 5 years; first three pages.
b.3.9. Optimize strategies and resources, to include minimum standards such that adequate laboratory and human resource capacity can be established to maintain quality integrated surveillance at scale.
Search strategy (grey literature, Google Scholar):
Cost AND capacity OR surveillance AND AMR OR AMU
Filter: Lat 5 years; first three pages.
b.3.10. Implement management options to prevent and address releases, effluent, and waste from intensive animal and crop production and from healthcare facilities and pharmaceutical manufacturing.
Search strategy (grey literature, Google Scholar):
Cost AND environment AND waste AND AMR OR AMU
Filter: Lat 5 years; first three pages.
b.3.11. Develop new methods/technologies to remove antimicrobial residues from the flows of wastewater, manure, and agricultural run-off.
Search strategy (grey literature, Google Scholar):
Cost AND residues AND AMR OR AMU
Filter: Lat 5 years; first three pages.
b.3.12. Develop soil/water/air-appropriate diagnostics.
Search strategy (grey literature, Google Scholar):
Cost AND diagnostic AND AMR OR AMU
Filter: Lat 5 years; first three pages.
b.4. Plants
b.4.1. Communicate with, educate, and provide training to farmers on AMR, integrated pest management (IPM), and the appropriate use and disposal of pesticides / herbicides/ molluscicides.
Search strategy (grey literature, Google Scholar):
Cost AND pesticide OR herbicide OR molluscicides AND AMR OR AMU
Filter: Lat 5 years; first three pages.
b.4.2. National surveillance of AMR data in food and agriculture and AMU data in crops through enrolling in the International FAO Antimicrobial Resistance Monitoring (InFARM).
Search strategy (grey literature, Google Scholar):
Cost AND surveillance OR data AND food OR agriculture AND AMR OR AMU
Filter: Lat 5 years; first three pages.
b.4.3. Incentivize farm assurance or certification benchmarking schemes in farms.
Search strategy (grey literature, Google Scholar):
Cost AND farm AND AMR OR AMU
Filter: Lat 5 years; first three pages.
b.4.4. Establish regional, central BSL (Biological Safety Level) 3 and 4 laboratories for detection of zoonotic and infectious diseases.
Search strategy (grey literature, Google Scholar):
Cost AND zoonotic AND laborator* AND AMR OR AMU
Filter: Lat 5 years; first three pages.
b.4.5. Reduce the secondary use of AMU as growth promoters in agriculture (e.g., avoid mention of this use on labels).
Search strategy (grey literature, Google Scholar):
Cost AND agriculture AND AMR OR AMU
Filter: Lat 5 years; first three pages.
b.4.6. Promote integrated pest management to reduce the use of antimicrobial pesticides.
Search strategy (grey literature, Google Scholar):
Cost AND pest AND AMR OR AMU
Filter: Lat 5 years; first three pages.
b.4.7. Reduce the need to use antimicrobial pesticides through the Reduce the Need for Antimicrobials on Farms (RENOFARM) initiative.
Search strategy (grey literature, Google Scholar):
Cost AND pesticides AND AMR OR AMU
Filter: Lat 5 years; first three pages.
b.5. Across sector interventions
b.5.1. Enhance policy, legislation, advocacy and financing.
Search strategy (grey literature, Google Scholar):
Cross-sectoral AND Cost AND policy OR legislation OR advocacy OR financing AND AMR OR AMU
Filter: Lat 5 years; first three pages.
b.5.2 Strengthen organisational development, implementation and sectoral integration.
Search strategy (grey literature, Google Scholar):
Cross-sectoral AND Cost AND Implement* OR development AND AMR OR AMU
Filter: Lat 5 years; first three pages.
b.5.3. Implement data, evidence, and knowledge.
Search strategy (grey literature, Google Scholar):
Cross-sectoral AND Cost AND data OR evidence AND AMR OR AMU
Filter: Lat 5 years; first three pages.
Appendix 5. Detailed information about the resources comprising the interventions
Table A5.1. Detailed information for each intervention included in the package
| Intervention | Specific component | Description | Source |
|---|---|---|---|
| 1. AMR awareness raising, education and behavior change of health workers and the community | 1. a. Enhance health worker training 1. b. Scale up mass media campaigns | 1. a A training program for health professionals to improve communication skills during consultations with their patients in outpatient care settings. 1. b. The modelled intervention is a nationwide mass media campaign involving mass media and social media platforms to raise AMR understanding and awareness across key stakeholders. | OECD (2023) |
| 2. Enhance food-handling practices / biosecurity practices to reduce the risk of AMR spread between humans and animals | 2. a. Improve food handling practices | A food safety control training program targets food service workers in food establishments, coupled with visual reminders and regular audits based on checklists. | OECD (2023) |
| 3. Research into new antimicrobials, diagnostics and vaccines for AMR and behavioral and implementation science | 3. a. New antibiotic incentive program | New antibiotic incentive program including 18 new antibiotics. | Towse and Silverman. Centre for Global Development (2022) |
| 4. Implementation of biosecurity measures to prevent the introduction and spread of disease in farms | 4. a. Improve farm hygiene | The modelled intervention is a procurement program that facilitates the purchase of PPE in farm settings by farmers and professional visitors like veterinarians. | OECD (2023) |
| 5. Implementation of infection, prevention, and control core components to mitigate AMR | 5. a. Enhance hand hygiene | A facility-based intervention that aims to enhance hand hygiene practices among health workers. | OECD (2023) |
| 6. Universal access to improved WASH and waste management to mitigate AMR | 6. a. Strengthen access to latrines and improved latrines | The intervention phase (community-led total sanitation) included bolstering access to latrines/improved latrines, etc. An improved latrine was defined as a pit-hole of 2 m depth or more, installation of a slab and a pit-hole cover, construction of a wall, door, and roof, and installation of a hand-washing facility with soap within the community-led total sanitation (CLTS) framework. | Cha S et al (2020) |
| 7. Ensure safe and sustainable disposal and treatment of antimicrobials and hazardous waste | 7. a. Enhance environmental hygiene | A bundled intervention that aims to enhance environmental hygiene practices in hospitals. | OECD (2023) |
| 8. Quality laboratory system and diagnostic stewardship to enable clinical bacteriology and mycology testing | 8. a. Implementation or scale up of Rapid diagnostic tests (RDTs) | A novel program aims to increase the use of rapid diagnostic tests by increasing the availability of point-of-care (POC) CRP in ambulatory care settings in combination with antibiotic treatment guidelines depending on the CRP levels. | OECD (2023) |
| 9. Access to vaccines and expanded immunization to manage AMR | 9. a. Improve vaccination coverage | Scale up of nationwide campaign of 23-valent pneumococcal polysaccharide (PVV23) targeting older adults. | Lu E (Yiwei) et al (2021) |
| 10. Up-to-date evidence-based treatment guidelines and antimicrobial stewardship programs | 10. a. Strengthening antimicrobial stewardship programs (ASPs) 10. b. Delayed antimicrobial prescribing 10. c. Financial incentives | 10. a. The modelled intervention entails scaling up a hospital-based program that involves the creation of multi-disciplinary teams that provide antibiotic stewardship and the scale-up of monitoring and surveillance systems. 10. b. The model intervention is the rollout of antimicrobial prescribing guidelines that promote delayed prescription in primary healthcare settings. 10. c A nationwide pay-for-performance (P4P) program that aims to optimize antimicrobial use in community settings by rewarding bonuses to prescribers for achieving pre-set antibiotic prescribing targets. | OECD (2023) |
Note. (*) New antibiotic intervention targets deaths due to E. Coli, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumanii, Pseudomonas aeruginosa, Streptococcus pneumoniae.
Appendix 6. Target coverage and impact data per intervention
Table A6.1. Target coverage values for each intervention included in the package
Intervention | Target coverage |
|---|---|
| 1. AMR awareness raising, education and behavior change of health workers and the community. | - Enhanced health worker training: 70% - Mass media campaigns: 100% |
| 2. Enhance food-handling practices / biosecurity practices to reduce the risk of AMR spread between humans and animals | 70% |
| 3. Quality laboratory system and diagnostic stewardship to enable clinical bacteriology and mycology testing. | 70% |
| 4. Access to vaccines and expanded immunisation to manage AMR. | 90% |
| 5. Up-to-date evidence-based treatment guidelines and antimicrobial stewardship programs. | - Strengthening antimicrobial stewardship programs (ASPs): 80% - Delayed antimicrobial prescription: 40% - Financial incentives: 70% |
| 6. Implementation of biosecurity measures to prevent the introduction and spread of disease in farms. | 70% |
| 7. Implementation of infection, prevention, and control (IPC) core components to mitigate AMR. | 70% |
| 8. Universal access to improved WASH and waste management to mitigate AMR. | 90% |
| 9. Ensure safe and sustainable disposal and treatment of antimicrobials and hazardous waste. | 70% |
| 10. Investment in new antimicrobials | 100% (*) |
(*) Assumption based on Towse and Silverman. Centre for Global Development (2022)
Table A6.2. Effectiveness data, population target, and impact for each intervention (and component) within the package
| Intervention | Specific component | Population target | Impact | Effectiveness value | Source |
|---|---|---|---|---|---|
| 1. AMR awareness raising, education and behavior change of health workers and the community | 1. a. Enhance health worker training | 1. a. Healthcare workers with impact on patients | 1. a. Resistant community infections | 1. a. 39% reduction in antibiotic prescription | OECD (2023) |
| 1. b. Scale up mass media campaigns | 1. b. Whole population | 1. b. Resistant community infections | 1. b. 7% reduction in antibiotic prescription | ||
| 2. Enhance food-handling practices / biosecurity practices to reduce the risk of AMR spread between humans and animals | 2. a. Improve food handling practices | Food caterers with impact on the population | Resistant and susceptible enteric infections | 28.6% reduction in microbial count | OECD (2023) |
| 3. Research into new antimicrobials, diagnostics and vaccines for AMR and behavioral and implementation science | 3. a. New antibiotic incentive program | Patients with resistant infections | Resistant set of infections | 5% reductions in deaths attributed to AMR each year: starting from year 10 onward (*) | Towse and Silverman. Centre for Global Development (2022) |
| 4. Implementation of biosecurity measures to prevent the introduction and spread of disease in farms | 4. a. Improve farm hygiene | Farmers with impact on the population | Resistant and susceptible community infections | 12% reduction in risk of infection among people who use personal protective equipment (PPE) compared to those who do not | OECD (2023) |
| 5. Implementation of infection, prevention, and control core components to mitigate AMR | 5. a. Enhance hand hygiene | Healthcare workers with impact on patients | Resistant and susceptible hospital infections | 33% reduction in risk of infection among people who comply with enhanced hand hygiene practices compared to those who do not | OECD (2023) |
| 6. Universal access to improved WASH and waste management to mitigate AMR | 6. a. Strengthen access to latrines and improved latrines | Children aged 0-5 | Resistant and susceptible enteric infections | 29% reduction in diarrhea cases | Assumption based on Cha S et al (2020) |
| 7. Ensure safe and sustainable disposal and treatment of antimicrobials and hazardous waste | 7. a. Enhance environmental hygiene | Healthcare workers with impact on patients | Resistant and susceptible hospital infections | 26% reduction in risk of infection among people who are exposed to enhanced environmental hygiene practices compared to those who do not | OECD (2023) |
| 8. Quality laboratory system and diagnostic stewardship to enable clinical bacteriology and mycology testing | 8. a. Implementation or scale up of Rapid diagnostic tests (RDTs) | Antibiotic prescribers in the community with impact on patients | Resistant community infections | 32% reduction in immediate antibiotic prescribing in adults and 46% in children < 18 years of age | OECD (2023) |
| 9. Access to vaccines and expanded immunization to manage AMR | 9. a. Improve vaccination coverage | Children aged 0-5 | Resistant and susceptible pneumococcal infections | Reduction in pneumococcal disease cases: - Pneumococcal pneumonia 9.41% reduction. - Pneumococcal meningitis: 42.46% reduction - Pneumococcal acute otitis media (AOM): 8.32% reduction | Lu E (Yiwei) et al (2021) |
| 10. Up-to-date evidence-based treatment guidelines and antimicrobial stewardship programs | 10. a. Strengthening antimicrobial stewardship programs (ASPs) 10. b. Delayed antimicrobial prescribing 10. c. Financial incentives | 10. a. ATB prescribers in hospitals with impact on patients 10. b. ATB prescribers in the community with impact on patients 10. c. ATB prescribers in the community with impact on patients | 10. a. Resistant hospital infections 10. b. Resistant community infections 10. c. Resistant community infections | 10. a. 25% reduction in antibiotic use 10. b. 60% reduction in antibiotic use 10. c. 8% reduction in antibiotic use | OECD (2023) |
Note. (*) New antibiotic intervention targets deaths due to E. Coli, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumanii, Pseudomonas aeruginosa, Streptococcus pneumoniae.
Appendix 7. Cost data for each intervention included in the package
Table A7.1. Cost data for each intervention included in the package
| Intervention | Specific component | Intervention costs | Original currency/year | Country/ region of reference | Source |
|---|---|---|---|---|---|
| 1. AMR awareness raising, education and behavior change of health workers and the community | 1. a. Enhance health worker training | 1. a. $0.40 per capita per year | 1. a. US$ PPP, 2020 | OECD countries | OECD (2023) |
| 1. b. Scale up mass media campaigns | 1. b. $0.69 per capita per year | 1. b. US$ PPP, 2020 | |||
| 2. Enhance food-handling practices / biosecurity practices to reduce the risk of AMR spread between humans and animals | 2. a. Improve food handling practices | $0.24 per capita per year | US$ PPP, 2020 | OECD countries | OECD (2023) |
| 3. Research into new antimicrobials, diagnostics and vaccines for AMR and behavioral and implementation science | 3. a. New antibiotic incentive program | $ 3.83 billion for total country’s costs for a 30-year period (*) | US$, 2020 | Japan | Towse and Silverman. Centre for Global Development (2022) |
| 4. Implementation of biosecurity measures to prevent the introduction and spread of disease in farms | 4. a. Improve farm hygiene | $0.245 per capita per year | US$ PPP, 2020 | OECD countries | OECD (2023) |
| 5. Implementation of infection, prevention, and control core components to mitigate AMR | 5. a. Enhance hand hygiene | $0.48 per capita per year | US$ PPP, 2020 | OECD countries | OECD (2023) |
| 6. Universal access to improved WASH and waste management to mitigate AMR | 6. a. Strengthen access to latrines and improved latrines | $ 45.80 per capita for a 10-year period | US$ PPP, 2016 | Ethiopia | Assumption based on Cha S et al (2020) |
| 7. Ensure safe and sustainable disposal and treatment of antimicrobials and hazardous waste | 7. a. Enhance environmental hygiene | $2.24 per capita per year | US$ PPP, 2020 | OECD countries | OECD (2023) |
| 8. Quality laboratory system and diagnostic stewardship to enable clinical bacteriology and mycology testing | 8. a. Implementation or scale up of Rapid diagnostic tests (RDTs) | $1.34 per capita per year | US$ PPP, 2020 | OECD countries | OECD (2023) |
| 9. Access to vaccines and expanded immunization to manage AMR | 9. a. Improve vaccination coverage | $0.21 per capita per year | US$ PPP, 2020 | OECD countries | OECD (2023) |
| 10. Up-to-date evidence-based treatment guidelines and antimicrobial stewardship programs | 10. a. Strengthening antimicrobial stewardship programs (ASPs) 10. b. Delayed antimicrobial prescribing 10. c. Financial incentives | 10. a. $2.3 per capita per year 10. b. $0.45 per capita per year 10. c. $2.58 per capita per year | 10. a. US$ PPP, 2020 10. b. US$ PPP, 2020 10. c. US$ PPP, 2020 | OECD countries | OECD (2023) |
Note (*) For this intervention, costs related to improve access to all three types -- Access, Watch, and Reserve antibiotics will also be considered. From the SECURE work, there is an estimate that it will cost approximately 44.3m US$ per 100m population using public health service.
Appendix 8. Regions included in the analysis
Table 8.1. Regions included in the analysis defined by WHO geographic regions and 2024 World Bank income categories
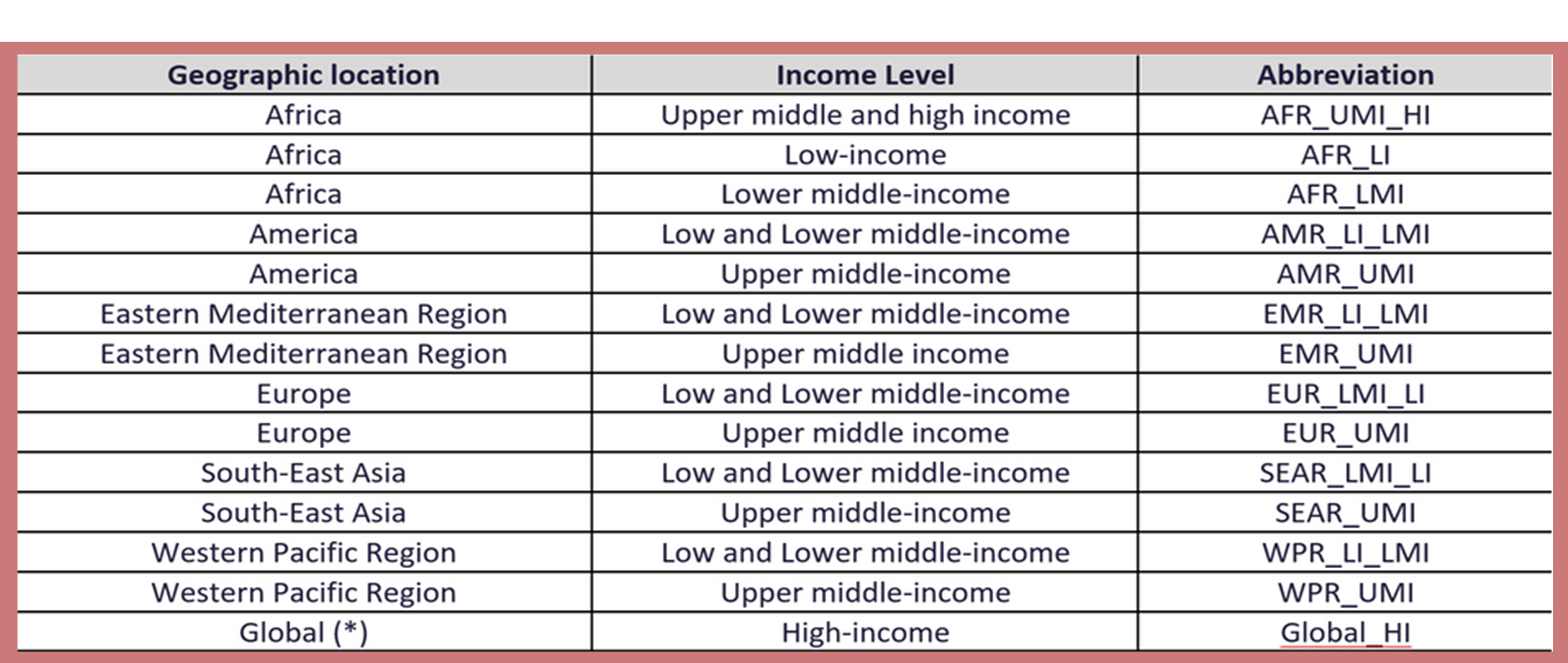
Note (*) Global (HIC) region includes all high-income countries across the globe except the African region.
References
1. OECD. Antimicrobial Resistance Tackling the Burden in the European Union Briefing note for EU/EEA countries Contents. 2019.
2. IHME. Antimicrobial Resistance (AMR). Available at: https://www.healthdata.org/research-analysis/health-risks-issues
3. The World Bank. Drug-Resistant Infections: A Threat to Our Economic future (March 2027). Available at: https://www.worldbank.org/en/topic/health/publication/drug-resistant-infections-a-threat-to-our-economic-future
4. OECD. The OECD Strategic Public Health Planning (SPHeP) for antimicrobial resistance [Internet]. 2022. Available from: http://oecdpublichealthexplorer.org/amr-doc/
5. WHO. Global Action Plan on Antimicrobial Resistance [Internet]. 2015 [cited 2023 Aug 7]. Available from: https://iris.who.int/bitstream/handle/10665/193736/9789241509763_eng.pdf?sequence=1
6. Quadripartite. One Health Joint Plan of Action, 2022–2026 [Internet]. One Health Joint Plan of Action, 2022–2026. FAO; UNEP; WHO; World Organisation for Animal Health (WOAH) (founded as OIE); 2022 Oct [cited 2023 Aug 7]. Available from: https://iris.who.int/bitstream/handle/10665/363518/9789240059139-eng.pdf?sequence=1
7. WHO. People-centred framework for addressing antimicrobial resistance in the human health sector Draft for public consultation ii. 2022.
8. Health and economic impacts of antimicrobial resistance in the Western Pacific Region, 2020–2030. 2023. Licence: CC BY-NC-SA 3.0 IGO. Available at: https://www.who.int/publications/i/item/9789290620112
9. Silverman Bonnifield T. Estimating Japan’s Return on Investment from an Ambitious Program to Incentivize New Antibiotics. 2022.
10. OECD. Embracing a One Health Framework to Fight Antimicrobial Resistance. Paris: OECD Publishing ; 2023.
11. OECD-WHO. Addressing the Burden of Infections and Antimicrobial Resistance Associated with Health Care [Internet]. 2022. Available from: https://www.oecd.org/health/Addressing-burden-of-infections-and-AMR-associated-with-health-care.pdf
12. Morel CM, Alm RA, Årdal C, Bandera A, Bruno GM, Carrara E, et al. A one health framework to estimate the cost of antimicrobial resistance. Antimicrob Resist Infect Control. 2020 Dec 1;9(1).
13. Sustaining Action Against Antimicrobial Resistance A CASE SERIES OF COUNTRY EXPERIENCES [Internet]. Washington, DC; [cited 2023 Aug 13]. Available from: https://openknowledge.worldbank.org/server/api/core/bitstreams/624f5193-99c0-5a28-adfe-0191a8c40d04/content
14. WHO. Global Antimicrobial Resistance and Use Surveillance System (GLASS) [Internet]. [cited 2023 May 30]. Available from: https://www.who.int/initiatives/glass
15. North J. Challenges to Tackling Antimicrobial Resistance: Economic and Policy Responses [Internet]. Anderson M, Cecchini M, Mossialos E, editors. Cambridge University Press; 2020 [cited 2023 Jul 30]. Available from: https://www.cambridge.org/core/product/identifier/9781108864121/type/book
16. OECD & WHO. Challenges to Tackling Antimicrobial Resistance. Cambridge University Press; 2019.
17. Evaluation Unit. Comprehensive Review of the WHO Global Action Plan on Antimicrobial Resistance Volume 1: Report WHO Evaluation Office. 2021.
18. Jit M, Ng DHL, Luangasanatip N, Sandmann F, Atkins KE, Robotham J V., et al. Quantifying the economic cost of antibiotic resistance and the impact of related interventions: Rapid methodological review, conceptual framework and recommendations for future studies. Vol. 18, BMC Medicine. BioMed Central Ltd.; 2020.
19. UNEP. Environmental Dimensions of Antimicrobial Resistance Summary for Policymakers [Internet] [Internet]. 2022. Available from: https://wedocs.unep.org/bitstream/handle/20.500.11822/38373/antimicrobial_R.pdf.
20. FAO. The FAO Action Plan on Antimicrobial Resistance 2021–2025 [Internet]. Rome, Italy; 2021. Available from: https://www.fao.org/documents/card/en/c/cb5545en
21. OECD. Stemming the Superbug Tide: Just A Few Dollars More [Internet] [Internet]. OECD Health Policy Studies, editor. OECD Publishing; 2018 [cited 2023 Jul 30]. Available from: https://www.oecd.org/health/stemming-the-superbug-tide-9789264307599-en.htm
22. Al-Haboubi M, Trathen A, Black N, Eastmure E, Mays N. Views of health care professionals and policy-makers on the use of surveillance data to combat antimicrobial resistance. BMC Public Health. 2020 Mar 2;20(1).
23. Ekiri A, Haesler B, Mays N, Staerk K, Mateus A. Impact of guidelines and recommendations on the level and patterns of antimicrobial use in livestock and companion animals SYSTEMATIC REVIEW [Internet]. 2019. Available from: www.rvc.ac.uk
24. Murphy D, Ricci A, Auce Z, Beechinor JG, Bergendahl H, Breathnach R, et al. EMA and EFSA Joint Scientific Opinion on measures to reduce the need to use antimicrobial agents in animal husbandry in the European Union, and the resulting impacts on food safety (RONAFA). EFSA Journal [Internet]. 2017 Jan;15(1). Available from: http://doi.wiley.com/10.2903/j.efsa.2017.4666
25. Ryan M. Evaluating the economic benefits and costs of antimicrobial use in food-producing animals. Vol. 132, OECD Food, Agriculture and Fisheries Papers. Paris; 2019.
26. FAO, VMD. Tackling antimicrobial use and resistance in food-producing animals: Lessons learned in the United Kingdom of Great Britain and Northern Ireland. Rome, Italy; 2022.
27. North J. Challenges to Tackling Antimicrobial Resistance: Economic and Policy Responses. Anderson M, Cecchini M, Mossialos E, editors. Cambridge: Cambridge University Press; 2020.
28. WHO. Leveraging Vaccines to Reduce Antibiotic Use and Prevent Antimicrobial Resistance: An Action Framework. 2020.
29. UNEP. Bracing for Superbugs: Strengthening environmental action in the One Health response to antimicrobial resistance [Internet]. Geneva; 2023 Feb. Available from: https://www.unep.org/resources/superbugs/environmental-action
30. Ananthakrishnan A, Painter C, Teerawattananon Y. A protocol for a systematic literature review of economic evaluation studies of interventions to address antimicrobial resistance. Syst Rev. 2021 Dec 1;10(1).
31. Naylor NR, Lines J, Waage J, Wieland B, Knight GM. Quantitatively evaluating the cross-sectoral and One Health impact of interventions: A scoping review and case study of antimicrobial resistance. Vol. 11, One Health. Elsevier B.V.; 2021.
32. Poudel AN, Zhu S, Cooper N, Little P, Tarrant C, Hickman M, et al. The economic burden of antibiotic resistance: A systematic review and meta-analysis. PLoS One. 2023 May 1;18(5 May).
33. Wubishet BL, Merlo G, Ghahreman-Falconer N, Hall L, Comans T. Economic evaluation of antimicrobial stewardship in primary care: a systematic review and quality assessment. Vol. 77, Journal of Antimicrobial Chemotherapy. Oxford University Press; 2022. p. 2373–88.
34. Painter C, Faradiba D, Chavarina KK, Sari EN, Teerawattananon Y, Aluzaite K, et al. A systematic literature review of economic evaluation studies of interventions impacting antimicrobial resistance. Antimicrob Resist Infect Control. 2023 Dec 1;12(1).
35. D’hulster E, Burghgraeve T De, Luyten J, Verbakel JY. Cost-effectiveness of point-of-care interventions to tackle inappropriate prescribing of antibiotics in high- and middle-income countries: a systematic review. Journal of Antimicrobial Chemotherapy. 2023 Apr;78(4):893–912.
36. Cuevas C, Batura N, Wulandari LPL, Khan M, Wiseman V. Improving antibiotic use through behaviour change: A systematic review of interventions evaluated in low- And middle-income countries. Vol. 36, Health Policy and Planning. Oxford University Press; 2021. p. 754–73.
37. Nathwani D, Varghese D, Stephens J, Ansari W, Martin S, Charbonneau C. Value of hospital antimicrobial stewardship programs [ASPs]: A systematic review. Vol. 8, Antimicrobial Resistance and Infection Control. BioMed Central Ltd.; 2019.
38. Silverman Bonnifield R and TA. An Ambitious USG Advanced Commitment for Subscription-Based Purchasing of Novel Antimicrobials and Its Expected Return on Investment. 2022.
39. Cha S, Jung S, Bizuneh DB, Abera T, Doh YA, Seong J, et al. Benefits and costs of a community-led total sanitation intervention in rural Ethiopia—A trial-based ex post economic evaluation. Int J Environ Res Public Health. 2020 Jul 2;17(14):1–21.
40. Lu E, Chen HH, Zhao H, Ozawa S. Health and
economic impact of the pneumococcal conjugate vaccine in hindering
antimicrobial resistance in China. Proceedings of the National Academy of
Sciences [Internet]. 2021;118(13). Available from: https://doi.org/10.1073/pnas.2004933118
